Almost every family has had a brush with cancer at some point, racking up millions of lives each year across the globe. Understanding the basics of carcinogenesis—the stepwise process by which normal cells turn cancerous—brings hope, helps reduce stigma, and empowers us all towards prevention and better treatment.
What Is cancer?
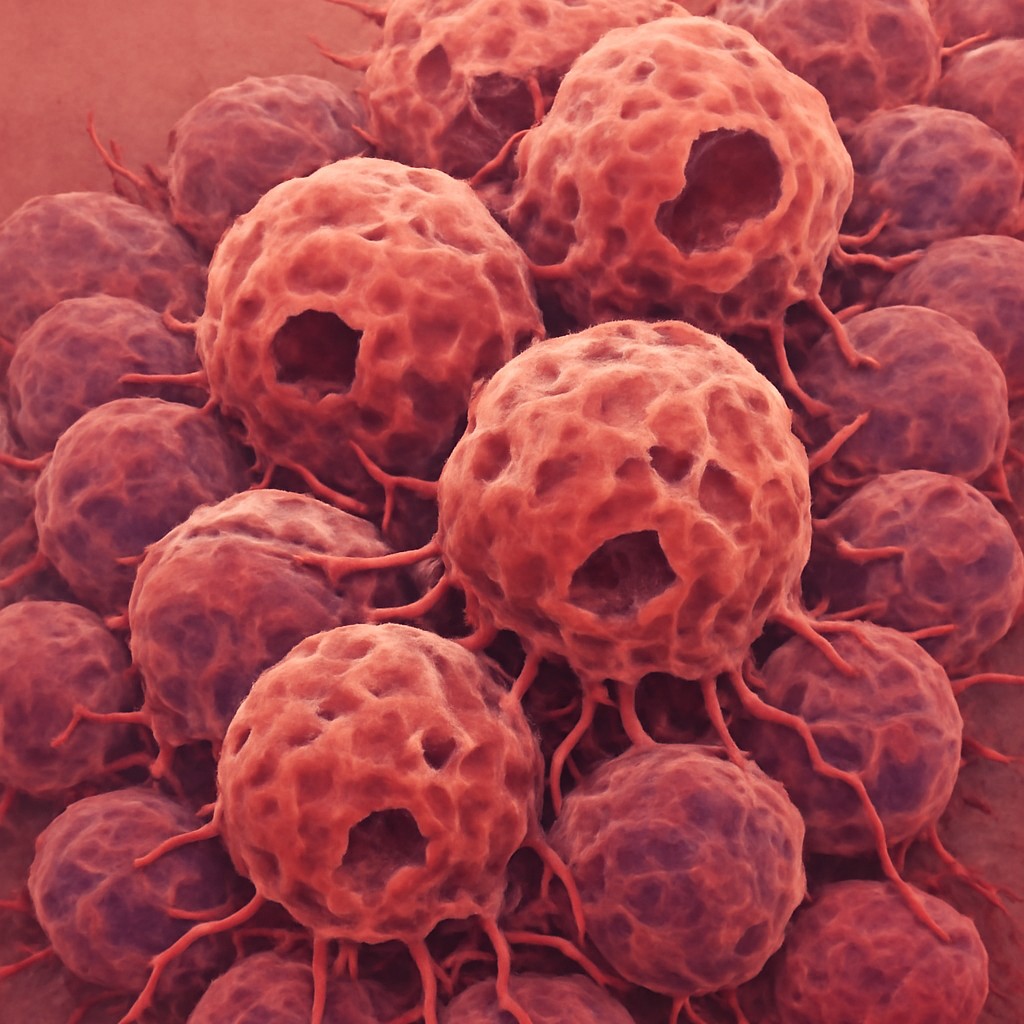
Cancer is, essentially, a disease that ensues when the body loses control. All the cells in our body are tightly regulated: they must know when to grow or stop, when to specialize, and ultimately, when to die off. Cancer totally disregards these rules. Its cells multiply without limit, stray further from their original form, and may invade other tissues far from their starting place, forming new tumors in distant organs (metastasis)1.
What makes cancer particularly complicated is that it’s not just one illness, but rather a combination of many. Each cancer type has different risk factors, symptoms, and treatment choices. Still, beneath all this diversity, cancers have shared origins and behaviors.
The global burden
The World Health Organization estimates that nearly one in six deaths worldwide is due to cancer, with more than 10 million people dying from it in 2020 alone. Certain cancers are more common in some regions; for instance, liver cancer burdens parts of Asia and Africa, while lung, breast, and colorectal tumors are more prevalent in Western countries2,3.
Cancer leaves deep social and economic scars. It not only takes lives, but also causes loss of income, long-term disability, and immense psychological stress on patients and families. Prevention and early detection, therefore, are not just medical advancements, they are very much a necessity.
Cancer as a genetic disease
For centuries, the cause of cancer was a mystery. But it has now been discovered that cancer is nothing, but a disease rooted in the genes of our cells. Nearly all cancers arise because of acquired mutations—changes in the DNA that occur during a person’s lifetime, not inherited from their parents.
Of course, some people do inherit genes that push them more at risk towards developing cancer, but these hereditary syndromes make up only about 5% of cases4. In most people, it’s the slow accumulation of errors in DNA over years—due to aging, environmental factors like chemicals or radiation, infections, or random chance, that eventually drives a cell to turn cancerous5.
The hallmarks of cancer
Modern research has described a set of “hallmarks”, traits that cancer cells reliably acquire and which can help us distinguish them from healthy ones6:
- They can keep dividing, even in the absence of normal growth signals.
- Unlike normal cells, which self-destruct when damaged, cancer cells evade this fate.
- Cancer ignores signals that should halt its growth.
- Tumors induce new blood vessels (angiogenesis) to secure their food supply.
- Malignant cells break away and colonize distant tissues.
- Cancer adapts its metabolism and can escape the immune system’s notice.
Recognizing these hallmarks helps us to find targeted ways to interrupt these malignant abilities.
The journey from healthy cells to cancer: carcinogenesis
How normal cells stay in line
In a healthy body, cells operate within strict rules:
- The cell cycle is tightly controlled by proteins (cyclins, CDKs) that act like green and red lights, ensuring cells only divide when appropriate7.
- Apoptosis (programmed cell death) is the body’s quality control, removing damaged or excess cells8.
- Differentiation and organization ensure cells take on specialized roles, forming coherent tissues and organs9, 10.
Disruption to any of these systems sets the stage for cancer.
Genes at the heart: oncogenes, tumor suppressors, and more
Cancer is fundamentally a disease of faulty, out-of-control genes. It is caused by both oncogenes—that accelerate cell growth when they shouldn’t, and tumor suppressor genes—whose job is to keep growth in check.
- Proto-oncogenes are normal genes that help cells grow; but when mutated, they transform into oncogenes, promoting uncontrolled cell growth and division11. For example, Ras, Myc and EGFR proteins lead to constitutive activation of growth and signaling pathways.
- Tumor suppressor genes such as TP53 or RB inhibit cell growth and division12. Usually, it requires loss of both of these gene copies to lead to development of cancer (Knudson’s“two-hit hypothesis”).
- DNA repair genes encode proteins essential for detecting and fixing damage13. Mutations in DNA repair genes lead to genomic instability, as seen in mutations of Mismatch Repair (MMR) genes such as MLH1, MSH2/6, which account for 2-5% of all colorectal cancers.
- Epigenetic changes, which are chemical modifications to DNA or its histone proteins—also play a key role, turning critical genes on or off without altering the underlying genetic code itself14. These changes, involving DNA methylation, histone modification and dysregulation of non-coding RNAs lead to genomic instability.
The path to cancer: from mutation to malignancy
The process of carcinogenesis unfolds in three broad stages15:
- Initiation: A single cell suffers a permanent, irreversible DNA change.
- Promotion: This mutated cell is induced to multiply—by hormones, chronic inflammation, or repeated exposure to promoting chemicals.
- Progression: As more errors accumulate, the cell’s descendants become truly malignant, gaining the power to invade and spread.
Triggers and risk factors for carcinogenesis
Cancer is caused by an interplay of triggers building up over time:
- Chemical carcinogens like those in tobacco smoke, alcohol, or certain industrial byproducts can directly or indirectly damage DNA16.
- Physical agents include ultraviolet light, and ionizing radiation from sources like X-rays, which significantly increase the risk of skin cancer17.
- Viral infections such as human papillomavirus (HPV), hepatitis B and C, and Epstein-Barr virus introduce genes into cells or promote chronic inflammation, both raising cancer risk18.
- Chronic infections by bacteria such as Helicobacter pylori that affect the stomach, or parasites including liver flukes or schistosomes that trigger persistent inflammation pose as a key risk for cancer in affected organs19, 20.
- Inherited syndromes caused by genes such as BRCA1/2 in breast and ovarian cancers, and APC in colon cancer mean that a person is already midway, or well-advanced, along the path to cancer21, 22.
- Lifestyle factors such as smoking, alcohol abuse, obesity, poor diet, and being physically inactive—all increase risk of developing cancer23.
Some people experience more than one risk factor, which makes prevention so much more urgent.
A look at major cancer types
Lung cancer continues to be the world’s deadliest form of cancer, with around one-third of cancer-related deaths resulting from tobacco use24. Air pollution and genetic susceptibility also play a role. Unfortunately, it’s often diagnosed late, after it has considerably spread.
Breast cancer is infamous for affecting women worldwide, though men can also rarely be affected. It is now well-known that family genes like BRCA1/2 is often an influencing factor25, 26. However, hormone exposure over a lifetime and other lifestyle factors can also play big roles.
Colorectal cancer often starts unnoticed as a benign polyp27. These invasive diseases result due to gradual accumulation of genetic mutations, many of which are preventable. Screening, using techniques like colonoscopy, is often highly effective at preventing this kind of cancer28.
Prostate cancer usually develops in older men29. It is influenced by age, testosterone, and sometimes inheritance. Some cases are slow and not life-threatening, while others are aggressive.
Leukemias and lymphomas are blood cancers that can strike at any age30, 31. There are certain types closely linked to infections or inherited mutations.
Liver cancer is common where previous cases of hepatitis B and C are common or where exposure to food contaminants such as aflatoxin is predominant32.
Pancreatic, ovarian, and brain cancers are less common but often deadly33–35. This is in part because they can progress without early symptoms and are difficult to detect.
Skin cancer, including melanoma, remains a leading cause of cancer36. These happen especially due to UV exposure, and so many are preventable with sun protection and vigilance.
Why understanding carcinogenesis matters
A deep understanding of how cancer develops has profoundly changed medicine. By unraveling the processes behind carcinogenesis, we are now able to prevent many cancers before they begin. Recognizing harmful exposures and risky behaviors has allowed for safer workplaces, healthier lifestyles, and the widespread use of vaccines against cancer-causing viruses, such as those for HPV and hepatitis B37, 38.
This knowledge also underpins the success of early detection. Cancer screening techniques, like mammograms and colonoscopies, advanced imaging technologies, and even artificial intelligence tools are increasingly being used to identify disease in its earliest, and most treatable stages, often before symptoms appear39-42.
Perhaps most remarkably, advances in the genetic and molecular roots of cancer, driven by multi-omics approaches have transformed treatment through precision medicine43, 44. Doctors can now tailor therapies to target specific weaknesses in an individual’s tumor, improving outcomes and minimizing side effects. Innovations such as immunotherapy—including CAR T-cell therapy, immune checkpoint inhibitors, therapeutic monoclonal antibodies, and oncolytic viruses, as well as emerging fields like theranostics and nanomedicine, all stem from this deeper understanding of carcinogenesis45-51. Additionally, disease modeling, including the use of organoids helps researchers predict cancer behavior and optimize treatment approaches52, 53.
In short, studying how cancer begins not only helps us prevent and detect the disease sooner but also fuels the development of more effective, less harmful treatments, changing the outlook for people worldwide.
The path forward
The numerous small missteps in DNA that give rise to cancer, influenced by the environment and chance, makes it a challenging opponent. Yet, this same complexity opens the door to numerous opportunities for prevention, smarter treatment, early detection, and, hopefully, cures, one day.
Today, with every new discovery, scientists and doctors are as close as ever to making cancer a manageable or even preventable disease. And while the fight continues, understanding the hidden logic of cancer’s origins is the first, and most hopeful step.