Regenerative medicine is a rapidly evolving field that is making a paradigm shift in the way we approach disease and injury. It brings forth interdisciplinary collaboration to address the root cause of tissue damage or organ failure, moving beyond merely managing symptoms. The core strategy is to leverage the body’s innate healing mechanisms or to introduce new biological components to repair, replace, and regenerate damaged cells, tissues, and entire organs, with the ultimate aim of restoring normal function1.
The human body has an extraordinary capacity to heal and renew itself, as happens when a simple cut on the finger seals itself, or a broken bone that knits back together. However, tissues like cartilage, nerve tissue, or heart muscle after a severe attack hardly undergo regeneration, and this is where regenerative medicine steps in. It offers hope to patients with significant trauma, chronic degenerative diseases like osteoarthritis or neurodegenerative disorders, or end-stage organ failure2-4. Such patients otherwise had to rely on lifelong medication, painful surgeries, or organ transplantation. And organ transplantation often has the limitation of donor shortages and the persistent risk of immune rejection5.
Types of regenerative medicine
A diverse array of sophisticated approaches aim to facilitate healing and restoration:
Cell-based therapies
Cell therapies are being explored to treat various kinds of conditions, including spinal cord injuries, heart disease, diabetes, neurological disorders like Parkinson’s, and various orthopedic injuries6.
Typically, the process involves isolating potent cells from the patient themselves or sometimes from an allogeneic donor, expanding them in a laboratory, and then carefully delivering them into the body to replace damaged tissue or organ. This helps to promote healing or modulate the local environment. Following are the different kinds of cells used for these kinds of therapies:
Stem cells
These are the foundational cells of the body having the remarkable ability to develop into many different cell types7. Among them, pluripotent stem cells, such as embryonic stem cells (ESCs), have the potential to become virtually any cell in the body. However, there are ethical concerns surrounding the use of ESCs.
Adult stem cells, such as mesenchymal stem cells from bone marrow or fat or hematopoietic stem cells from bone marrow or cord blood, are also sometimes used due to their valuable anti-inflammatory and immunomodulatory properties. However, they are multipotent in nature, meaning they can differentiate into only a limited range of cell types within a specific lineage.
Nowadays, adult cells, such as skin cells, are reprogrammed by inducing genes and factors to be pluripotent. These cells, known as induced pluripotent cells (iPSCs), offer a promising ethical alternative to ESCs for patient-specific therapies, and they can also be made to bypass immune rejection.
Progenitor cells
These cells are more specialized than stem cells but can still differentiate, and are often committed to a particular cell lineage8.
Differentiated cells
In a few specific cases, fully differentiated cells are implanted directly, such as the implantation of chondrocytes for cartilage repair9.
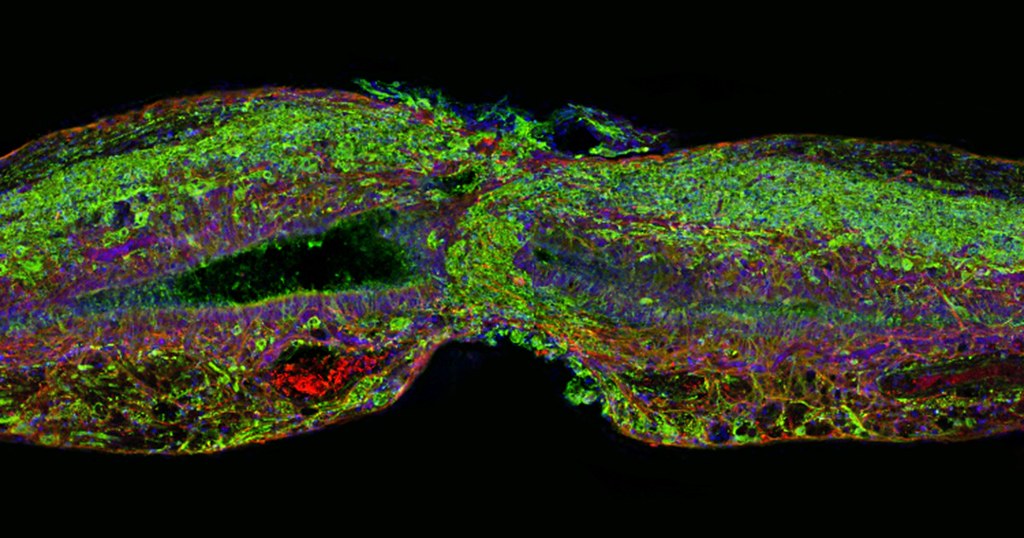
Tissue engineering and biomaterials
Tissue engineering creates functional tissues or even rudimentary organs through the use of sophisticated scaffolds and growth factors10. Scaffolds, derived from natural sources like collagen or fibril, or synthesized from biocompatible polymers, provide the necessary structural support to these constructs. These constructs can be grown in a lab for later implantation or designed to guide regeneration directly within the body. Examples range from growing skin grafts for burn victims to cartilage for joint repair11. This also includes the development of organoids, which are miniature, simplified versions of organs grown in vitro, offering powerful models for disease study and drug screening, and potentially for future transplantation.
Growth factors offer crucial biochemical signals to encourage the body’s native cells to migrate into these scaffolds and to proliferate, differentiate, and mature into the desired tissue. Often, patient-specific cells are also seeded onto these scaffolds to reinforce the formation of the tissue. Scaffolds are designed to biodegrade as the new tissue forms.
To construct complex, anatomically accurate tissue structures, 3D bioprinting is often employed, which uses specialized printers to deposit layers of cells and biomaterials in precise patterns12.
Gene therapy and gene editing
Gene therapy involves modifying or introducing genetic material into cells to enhance the body’s intrinsic regenerative capacity. It can be used not only to treat genetic disorders and certain cancers, but also to enhance tissue repair. This is achieved by delivering new genes that code for therapeutic proteins or growth factors to stimulate tissue repair, or by using CRISPR-Cas9 to precisely edit faulty genes responsible for inherited diseases or to reprogram cells into a desired type13,14.
Platelet-rich plasma (PRP) and growth factors
This approach, which is usually employed to treat tendon, ligament, and cartilage injuries as well as in chronic wound healing and dermatology, utilizes platelet-rich plasma15. PRP is derived from a patient’s own blood after concentrating the platelets in it.
These platelets, when activated, release a rich cocktail of growth factors that promote cell proliferation, tissue repair, and reduce inflammation. In order to directly stimulate cell growth, differentiation, and promote angiogenesis crucial for tissue health, specific growth factors, such as VEGF, FGF, and BMPs, can be delivered alone or in combination with other therapies.
The promise and the perils
Regenerative medicine offers the promise of curing or truly restoring function to damaged tissues and organs. This potentially eliminates the need for organ transplantation entirely. Consequently, two critical challenges are addressed: the severe shortage of organs available for transplant and the complex, lifelong drug regimens (including immunosuppressants) post-transplant patients must endure. By alleviating these burdens, regenerative medicine can significantly improve a patient’s quality of life and foster greater independence.
However, the field faces several challenges:
- Cell-based therapies using pluripotent stem cells face the issue of tumorigenicity16. So, it becomes essential to ensure that cells differentiate only into the desired tissue type.
- Efficacy and variability also remain critical hurdles5. It is difficult to ensure that transplanted cells survive, integrate, and function effectively within the complex host environment. This demands an ongoing effort to standardize protocols for consistent results.
- The regulatory and ethical landscape of regenerative medicine is also complex and evolves continually17-18. This is to ensure rigorous scientific validation, distinguishing legitimate therapies from unproven, and potentially harmful, treatments offered by unscrupulous clinics.
- Individualized regenerative therapies suffer from the challenges of scalability, and hence are not yet affordable for mass adoption19.
The horizon of healing
The field of regenerative medicine is rapidly advancing despite the challenges it faces. This is largely fueled by the integration of a number of cutting-edge technologies:
- Nanotechnology for targeted delivery and advanced scaffolds20.
- Robotics for automated manufacturing21.
- Microrobots and nanorobots for precise cell placement and the construction of 3D-bioprinted scaffolds and organoids22.
- Artificial intelligence for optimizing cell culture and predicting outcomes23.
Research is ongoing to refine cell sources and develop new methods for their manipulation, with a major focus on in situ regeneration24. These strategies stimulate the body’s own cells to repair damaged tissue without needing external cell transplantation.
Nevertheless, the ultimate goal of regenerative medicine is to achieve seamless biomimicry—designing materials and tissues that precisely replicate the intricate structure and function of natural biological systems.
As clinical translation progresses through rigorous trials, regenerative medicine promises definitive solutions for widespread organ failure and chronic degenerative diseases like Alzheimer’s and Parkinson’s. By tapping into the inherent capacity for repair and renewal, this field ushers in a future of renewed health and enhanced quality of life for countless individuals.