Photoacoustic imaging (PAI), also known as optoacoustic imaging, is a promising hybrid imaging modality that combines the strengths of optical and ultrasound imaging. The origins of PAI date back to 1880, with Alexander Graham Bell and Charles Sumner Tainter’s discovery of the photoacoustic effect. It leverages the rich contrast of optical imaging with the deep tissue penetration and spatial resolution of ultrasound. This dual capability enables it to capture both structural and functional information from biological tissues in real time.
Traditional optical imaging methods such as diffusive optical imaging (DOI) provide functional data without invasive procedures but are limited by poor spatial resolution. On the other hand, magnetic resonance imaging (MRI) and computed tomography (CT) offer high-resolution images but require large, expensive equipment, while techniques like positron emission tomography (PET) expose patients to ionizing radiation. PAI overcomes these drawbacks, providing a non-ionizing, high-resolution, and versatile imaging solution suitable for various clinical applications.
Fundamentals of photoacoustic imaging
In PAI, short pulses of light irradiate biological tissues, where specific molecules absorb the energy and generate a rapid thermal expansion, producing ultrasound waves. These waves carry vital information about the optical absorption properties of the tissue.
An ultrasound transducer (USTR) detects the photoacoustic signals, which then undergo signal processing, image reconstruction, and image processing procedures to generate cross-sectional two-dimensional or three-dimensional images revealing both the structure and function of tissue.
Different tissue components absorb light at different wavelengths. For example, in the ultraviolet spectrum, nucleic acids and aromatic amino acids are strong absorbers, while hemoglobin absorbs strongly in the visible and near-infrared spectrum.
Thus, PAI can visualize a wide variety of endogenous chromophores like DNA, melanin, and collagen, or utilize exogenous agents like indocyanine green (ICG) to enhance contrast. Depending on the clinical need, PAI can operate in various spectral ranges to target specific biomarkers.
Types of clinical photoacoustic imaging systems
Three major system configurations support diverse clinical applications:
- Dual-modal PAUSI systems integrate photoacoustic (PA) and ultrasound imaging (USI). These can be handheld or endoscopic, making them familiar and adaptable tools in clinical environments. The added advantage of providing optical biomarker data such as oxygen saturation and molecular tracer dynamics makes them suitable for imaging of skin, thyroid, breast, and limbs.
- Station-based tomographic PAI systems employ ring or hemispherical USTR arrays to detect omnidirectional photoacoustic waves. These systems provide deeper penetration (up to 5 cm) and are ideal for imaging larger regions like the brain or breast.
- Mesoscopic and microscopic PAI systems use high-frequency single-element USTRs for fine-resolution imaging. These systems are very useful in dermatology, where micron-scale detail is essential for diagnosing skin cancers or inflammatory conditions.
Organ- and system-specific applications
Integumentary system
Photoacoustic imaging is particularly well-suited for skin imaging due to the skin’s accessibility and natural optical contrast. It can assess melanoma depth (Breslow depth) noninvasively, with high accuracy. PAI has also been used to distinguish between benign and malignant skin lesions based on vascular biomarkers.
In psoriasis, PAI enables objective assessment of subsurface structures and helps to track improvement during treatment. This helps to find strong correlation between disease severity and patient-reported quality-of-life indices.
Musculoskeletal system
Photoacoustic imaging enables visualization of joints, tendons, and bones with high clarity. This can potentially help in evaluating muscle degeneration in disorders like Duchenne muscular dystrophy (DMD). While MRI is also used in DMD, it is less suitable for children and lacks molecular specificity. PAI, on the other hand, can differentiate collagen content and hemoglobin levels with statistical significance between patients and healthy individuals.
Cardiovascular system
Photoacoustic imaging provides insights into microvascular health, especially valuable in conditions like peripheral artery disease (PAD). PAI helps to measure oxygenated hemoglobin levels efficiently, allowing the determination of the three clinical stages of PAD. It can also reveal microvascular abnormalities in a way not possible with standard Doppler ultrasound. PAI can distinguish the different types of vascular malformations and can identify lipid-rich plaques in the arterial lumen of patients with carotid atherosclerosis, aiding stroke risk assessment.
Lymphatic system
Using contrast agents like ICG, PAI visualizes lymphatic vessels and nodes with remarkable spatial resolution. It also offers superior mapping of lymphatic architecture in comparison with near-infrared fluorescence imaging. PAI can effectively detect sentinel lymph nodes in breast cancer and melanoma patients, and the accuracy of such detection in clinical trials matched or exceeded conventional radiotracer methods.
Nervous system
PAI can be used to distinguish healthy individuals from patients with spinal muscular atrophy based on spectral signatures. In brain imaging, PAI offers direct quantitative assessment of brain oxygen saturation and cerebral blood volume. This is unlike blood-oxygen-level-dependent (BOLD) functional MRI (fMRI), which provides only relative measures of brain activity. PAI also yields remarkable brain vessel images and significantly improves temporal resolution for identifying functional brain activation compared to fMRI.
Endocrine system
PAI effectively evaluates thyroid disorders and distinguishes between benign and malignant nodules using hemoglobin and fat content metrics. In diabetes diagnostics, it can identify dermal biomarkers linked to microangiopathy and systemic disease progression.
Gastrointestinal system
In inflammatory bowel diseases like Crohn’s disease and ulcerative colitis, PAI can differentiate between active disease and remission through noninvasive measurement of hemoglobin levels in the intestinal wall. Its multispectral capacity offers quantitative assessment superior to traditional methods.
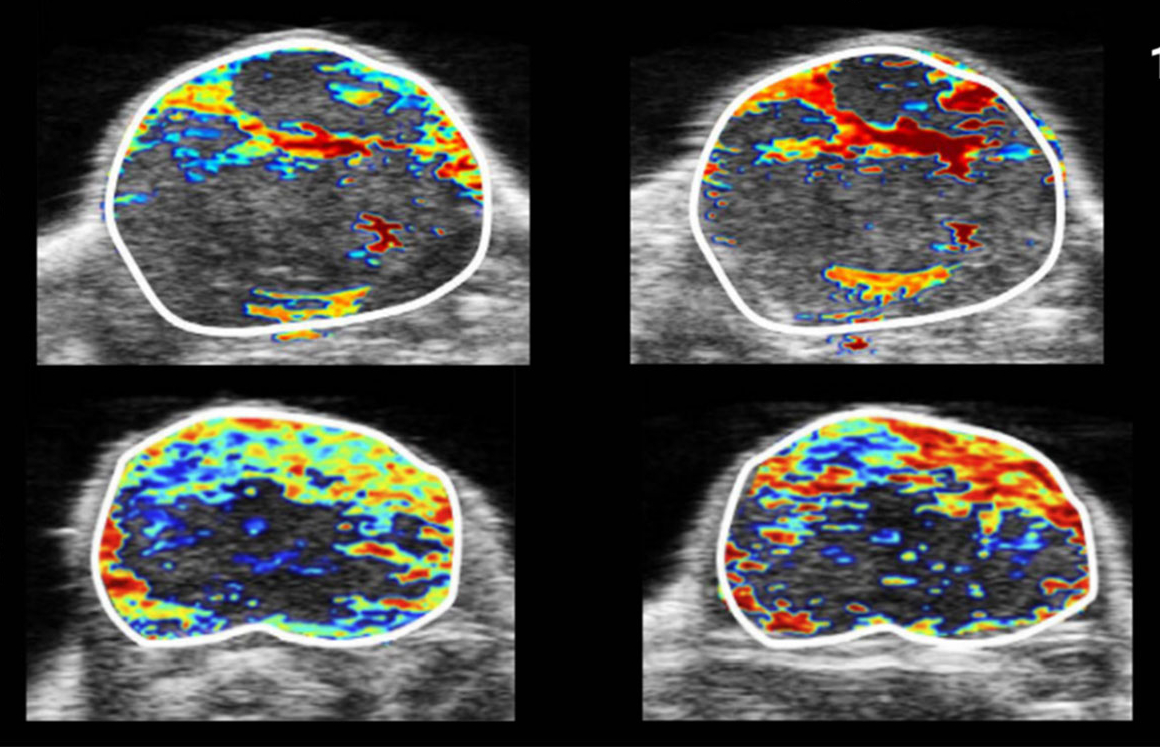
Reproductive system
Transrectal PAUSI is augmenting prostate cancer detection by combining anatomical ultrasound with hemoglobin and ICG-based optical contrast. This approach improves localization and characterization of tumors, potentially reducing reliance on MRI or PET.
Challenges in clinical translation
Despite its promise, PAI faces several challenges:
Technical barriers
Photoacoustic imaging suffers from limited light penetration and heterogeneous optical distribution, which complicates imaging depth and accuracy.
Limitations of USTR, such as narrow angle-of-view and bandwidth, affect image quality. Innovations such as optically transparent USTRs and optical sensors like Fabry Pérot interferometers offer potential solutions.
Industrial barriers
Photoacoustic imaging systems are expensive and require regular maintenance. For broader adoption, cost-effective components like pulsed laser diodes and LEDs must be optimized. Robust engineering and service infrastructure are also crucial for the reliability of PAI in clinical settings.
Ethical and accessibility concerns
The accuracy of a PAI measurement depends on skin color or melanin content, and this raises the key question on the equitable access and diagnostic reliability of PAI to diverse populations.
There is an ongoing debate about how much personal data (e.g., hormonal or reproductive indicators) should be collected and how such data might influence patient care or perceptions.
Standardization and regulatory pathways
To address these issues, the International Photoacoustic Standardization Consortium (IPASC) was established in 2019. IPASC promotes reproducibility, data sharing, and common standards across the global research community.
PAI’s regulatory journey has now commenced with full force. The FDA has granted premarket approval to the Imagio® Breast Imaging system after large-scale clinical trials. Similarly, CE-marked systems like MSOT and Japanese-approved platforms like LME-01 are expanding PAI’s footprint across various medical domains.
Outlook
PAI is poised to become a routine clinical imaging tool due to its demonstrated utility in diverse organ systems. Hardware innovations, like broadband USTRs and miniaturized laser fiber bundles, combined with software advancements in spectral unmixing and artifact suppression, are improving image quality and addressing concerns of affordability. The integration of artificial intelligence in automating image interpretation promises to improve diagnostic precision and reduce the workload of clinicians.
Recent milestones—including FDA approval, DICOM integration, and CPT code assignment—indicate that the potential of PAI is gradually becoming a reality. Going forward, as technical, industrial, and ethical hurdles get addressed through coordinated international efforts, PAI will become a reality in clinical setups with its powerful capabilities in viewing and diagnosing diseases.
Reference
Park, J., Choi, S., Knieling, F., et al. (2024). Clinical translation of photoacoustic imaging. Nature Reviews Bioengineering, 3, 193–212.
Image source
Rich, L. J., & Seshadri, M. (2016). Photoacoustic monitoring of tumor and normal tissue response to radiation. Scientific reports, 6(1), 21237.